Neurologic diseases that cause female urinary retention

Objective: The pathogenesis of female urinary retention is not well known. Hence, we systematically investigated the frequency of diseases that underlie female urinary retention in a urodynamic laboratory.
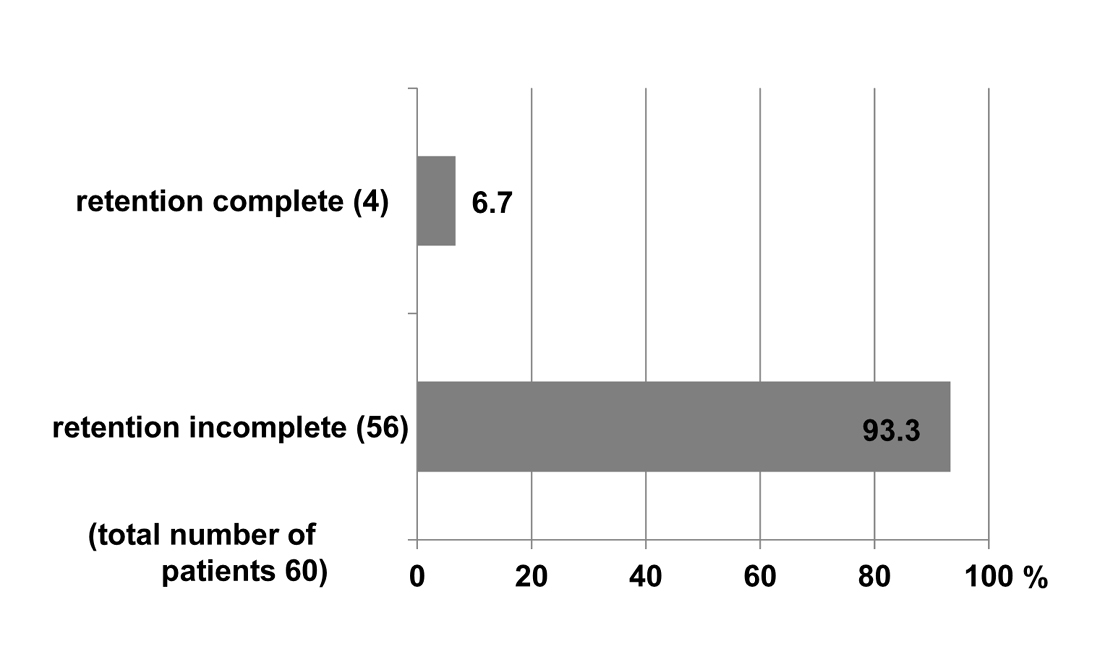
Methods: We analyzed data from 450 consecutive female patients. Data registries included the diagnosis, lower urinary tract symptom questionnaires, urodynamic study results, and neurologic exam observations. Complete urinary retention is defined as mean post-void residual (PVR) urine volume > 100 ml with no voluntary void at all; whereas incomplete urinary retention is defined as mean PVR urine volume > 100 ml after voluntary partial void.
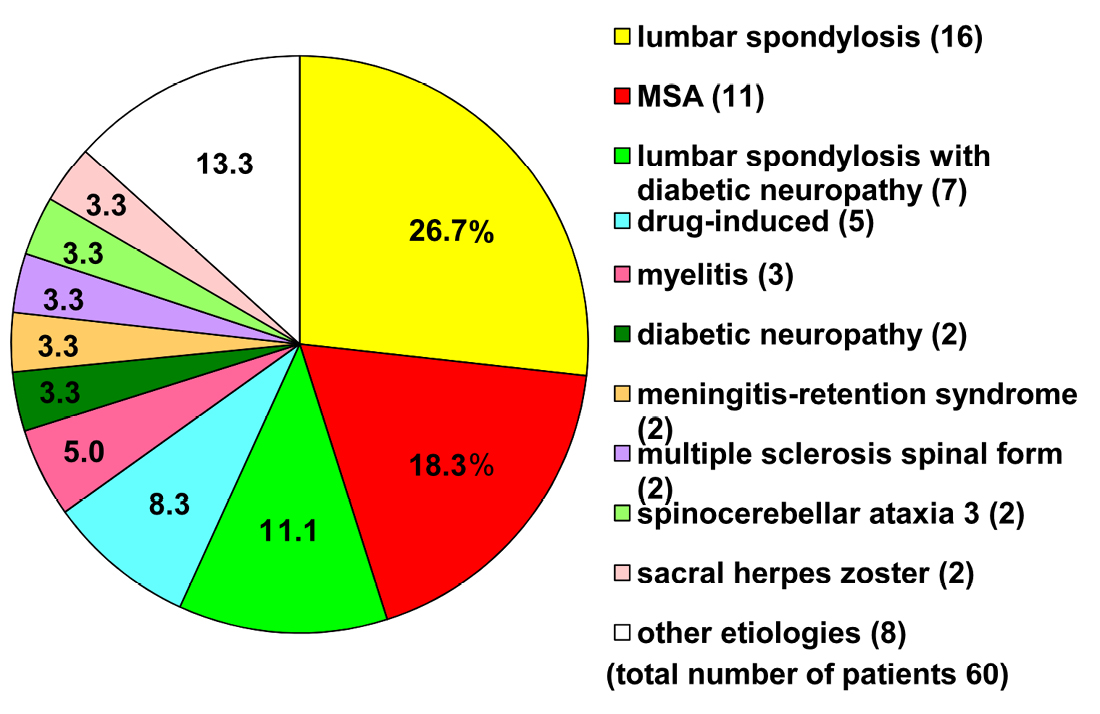
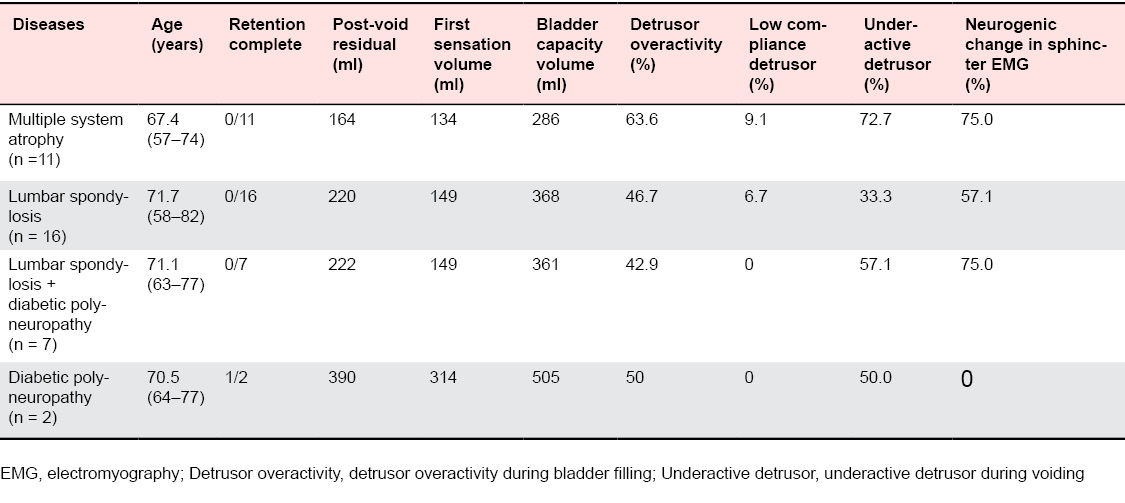
Results: Sixty of the 450 female patients visiting our lab (13%) had urinary retention with 4 (6.7%) of these having complete retention and 56 (93.3%) having incomplete retention. The most common underlying disease in these 60 patients was lumbar spondylosis (LS), 38.3% (with 16 patients having LS alone and 7 having LS & diabetic distal polyneuropathy [DPN]), multiple system atrophy (MSA), 18.3%, and DPN, 14.4% (with 2 patients having DPN alone and 7 having LS & DPN), followed by drug-induced retention (e.g., by antidepressants), 8.3%, acute myelitis of possible demyelinating origin, 5.0%, and other etiologies. An underactive detrusor was the major urodynamic findings in those patients.
Conclusion: The present study revealed that common etiologies for female urinary retention are neurologic, e.g., an underactive detrusor due to MSA, age-related LS, and lifestyle-related DPN. Therefore LS and DPN, both common diseases, should also become major treatment targets in order to maximize patients’ quality of life.
Introduction
Materials and Methods
LUTS questionnaires
Urodynamic studies
Neurologic and other examinations
Results
Discussion
- Robinson D, Staskin D, Laterza RM, Koelbl H (2012) Defining female voiding dysfunction: ICI-RS 2011. Neurourol Urodyn 31: 313-316. doi: https://doi.org/10.1002/nau.22213. [View Article] [PubMed] [Google Scholar]
- Hindley RG, Brierly RD, McLarty E, Harding DM, Thomas PJ (2002) A qualitative ultrastructural study of the hypocontractile detrusor. J Urol 168: 126-131. [PubMed] [Google Scholar]
- Osman NI, Chapple CR (2013) Fowler's syndrome--a cause of unexplained urinary retention in young women?. Nat Rev Urol 11: 87-98. doi: https://doi.org/10.1038/nrurol.2013.277. [View Article] [PubMed] [Google Scholar]
- Sakakibara R, Hattori T, Uchiyama T, Kamura K, Yamanishi T (2003) Uroneurological assessment of spina bifida cystica and occulta. Neurourol Urodyn 22: 328-334. doi: https://doi.org/10.1002/nau.2150. [View Article] [PubMed] [Google Scholar]
- Hiraga A, Sakakibara R, Mori M, Yamanaka Y, Ito S, et al. (2006) Urinary retention can be the sole initial manifestation of acute myelitis. J Neurol Sci 251: 110-112. doi: https://doi.org/10.1016/j.jns.2006.09.010. [View Article] [PubMed] [Google Scholar]
- Yamanishi T, Yasuda K, Sakakibara R, Hattori T, Uchiyama T, et al. (1998) Urinary retention due to herpes virus infections. Neurourol Urodyn 17: 613-619. [PubMed] [Google Scholar]
- Sakakibara R, Kishi M, Tsuyusaki Y, Tateno A, Tateno F, et al. (2012) "Meningitis-retention syndrome": a review. Neurourol Urodyn 32: 19-23. doi: https://doi.org/10.1002/nau.22279. [View Article] [PubMed] [Google Scholar]
- Wenning GK, Krismer F (2013) Multiple system atrophy. Handb Clin Neurol 117: 229-241. doi: https://doi.org/10.1016/B978-0-444-53491-0.00019-5. [View Article] [PubMed] [Google Scholar]
- Sakakibara R, Yamamoto T, Uchiyama T, Liu Z, Ito T, et al. (2005) Is lumbar spondylosis a cause of urinary retention in elderly women?. J Neurol 252: 953-957. doi: https://doi.org/10.1007/s00415-005-0790-3. [View Article] [PubMed] [Google Scholar]
- Tsai CH, Chou EC, Chou LW, Chen YJ, Chang CH, et al. (2010) The evaluation of bladder symptoms in patients with lumbar compression disorders who have undergone decompressive surgery. Spine 35: 849-854. doi: https://doi.org/10.1097/BRS.0b013e3181d55ad8. [View Article] [PubMed] [Google Scholar]
- Yamaguchi C, Sakakibara R, Uchiyama T, Yamamoto T, Ito T, et al. (2007) Overactive bladder in diabetes: a peripheral or central mechanism?. Neurourol Urodyn 26: 807-813. doi: https://doi.org/10.1002/nau.20404. [View Article] [PubMed] [Google Scholar]
- Shimizu T, Tokuda Y (2011) Acute urinary retention. Intern Med 50: 2255. [PubMed] [Google Scholar]
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, et al. (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 21: 167-178. [PubMed] [Google Scholar]
- Sakakibara R, Uchiyama T, Yamanishi T, Kishi M (2008) Sphincter EMG as a diagnostic tool in autonomic disorders. Clin Auton Res 19: 20-31. doi: https://doi.org/10.1007/s10286-008-0489-5. [View Article] [PubMed] [Google Scholar]
- Fowler CJ, Dalton C, Panicker JN (2010) Review of neurologic diseases for the urologist. Urol Clin North Am 37: 517-526. doi: https://doi.org/10.1016/j.ucl.2010.07.004. [View Article] [PubMed] [Google Scholar]
- Wheeler Jr, J.S. , Culkin DJ, Walter JS, Flanigan RC (1990) Female urinary retention. Urology 35: 428-432. [PubMed] [Google Scholar]
- Erdogan MO, Yıldız H, Artan S, Solak M, Taşcıoğlu F, et al. (2010) Association of estrogen receptor alpha and collagen type I alpha 1 gene polymorphisms with bone mineral density in postmenopausal women. Osteoporos Int 22: 1219-1225. doi: https://doi.org/10.1007/s00198-010-1312-4. [View Article] [PubMed] [Google Scholar]
- Perner A, Andersen JT, Juhler M (1997) Lower urinary tract symptoms in lumbar root compression syndromes: a prospective survey. Spine (Phila Pa 1976) 22: 2693-2697. [PubMed] [Google Scholar]
- Tsai CH, Chou ECL, Chou LW, Chen YJ, Chang CH, et al. (2010) The evaluation of bladder symptoms in patients with lumbar compression disorders who have undergone decompressive surgery. Spine 35: 849-854. doi: https://doi.org/10.1097/BRS.0b013e3181d55ad8. [View Article] [PubMed] [Google Scholar]
- Inui Y, Doita M, Ouchi K, Tsukuda M, Fujita N, et al. (2004) Clinical and radiologic features of lumbar spinal stenosis and disc herniation with neuropathic bladder. Spine (Phila Pa 1976) 29: 869-873. [PubMed] [Google Scholar]
- Sylvester PA, McLoughlin J, Sibley GN, Dorman PJ, Kabala J, et al. (1995) Neuropathic urinary retention in the absence of neurological signs. Postgrad Med J 71: 747-748. [PubMed] [Google Scholar]
- Hidmark A, Fleming T, Vittas S, Mendler M, Deshpande D, et al. (2014) A new paradigm to understand and treat diabetic neuropathy. Exp Clin Endocrinol Diabetes 122: 201-207. doi: https://doi.org/10.1055/s-0034-1367023. [View Article] [PubMed] [Google Scholar]
- Mastri AR (1980) Neuorpathology of diabetic neuropathic bladder. Ann Intern Med 92: 316-318. [PubMed] [Google Scholar]
- Van Poppel H, Stessens R, Van Damme B, Carton H, Baert L (1988) Diabetic cystopathy: neuropathological examination of urinary bladder biopsies. Eur Urol 15: 128-131. [PubMed] [Google Scholar]
- Yoshimura N, Chancellor MB, Andersson KE, Christ GJ (2005) Recent advances in understanding the biology of diabetes-associated bladder complications and novel therapy. BJU International 95: 733-738. doi: https://doi.org/10.1111/j.1464-410X.2005.05392.x. [View Article] [PubMed] [Google Scholar]
- Sakakibara R (2015) Lower urinary tract dysfunction in patients with brain lesions. Handb Clin Neurol 130: 269-287. doi: https://doi.org/10.1016/B978-0-444-63247-0.00015-8. [View Article] [PubMed] [Google Scholar]
- Panicker JN, Fowler CJ (2015) Lower urinary tract dysfunction in patients with multiple sclerosis. Handb Clin Neurol 130: 371-381. doi: https://doi.org/10.1016/B978-0-444-63247-0.00021-3. [View Article] [PubMed] [Google Scholar]
- Schurch B, Tawadros C, Carda S (2015) Dysfunction of lower urinary tract in patients with spinal cord injury. Handb Clin Neurol 130: 247-267. doi: https://doi.org/10.1016/B978-0-444-63247-0.00014-6. [View Article] [PubMed] [Google Scholar]
- Fowler CJ, Panicker JN, Drake M, Harris C, Harrison SCW, et al. (2009) A UK consensus on the management of the bladder in multiple sclerosis. Postgrad Med J 85: 552-559. doi: https://doi.org/10.1136/jnnp.2008.159178. [View Article] [PubMed] [Google Scholar]
- Sakakibara R, Panicker J, Finazzi-Agro E, Iacovelli V, Bruschini H (2015) A guideline for the management of bladder dysfunction in Parkinson's disease and other gait disorders. Neurourol Urodyn doi: https://doi.org/10.1002/nau.22764. [View Article] [PubMed] [Google Scholar]